Implant failure isn’t just a surgical concern—it’s a reputational, clinical, and financial risk. Understanding why implants fail, how to detect early signs, and what corrective options exist empowers dental professionals to improve outcomes and reduce avoidable complications. This guide explores the most common causes and solutions to ensure long-term implant success.
A failed dental implant typically means loss of stability, persistent pain or infection, or the need for removal or replacement. Common causes include poor osseointegration, peri-implantitis, mechanical overload, or prosthetic misfit. Early detection and structured maintenance reduce failure risks.
Dental implants can fail for various reasons, but not every issue qualifies as failure. A failed implant typically means it no longer supports the restoration, causes pain or infection, or requires removal or remake. Understanding the types of failure helps clinics manage patient expectations and plan appropriate solutions
Types of implant failure
Implant failure is typically categorized by timing. Early failure often occurs before restoration, while late failure happens after loading.
Osseointegration is the foundation of implant success. When bone doesn’t integrate with the implant surface, failure is inevitable.
| Sign | Implication |
|---|---|
| Radiolucent gap around implant | Indicates failed bone integration |
| Persistent discomfort or mobility | Suggests instability |
| Lack of progressive bone fill post-placement | Implies interrupted healing |
Even when integrated, an implant may still be considered a failure if it compromises function or appearance.
Sometimes, retreatment is the only option. Knowing when to remake saves time, cost, and reputation.
Understanding implant failure types allows teams to act early, improve communication, and avoid escalation.
Talk to Raytops Dental Lab to support remake coordination, digital scans, and fit analysis when rework becomes necessary.
Understanding the root causes of implant failure helps clinics plan better, prevent complications, and manage risk. While failure can result from many factors, some patterns appear consistently in both early and late-stage cases.

Causes of implant failure
Mechanical success starts at placement. If the implant lacks primary stability, integration is unlikely.
This is a leading cause of late implant failure. Inflammation leads to progressive bone loss and eventual destabilization.
| Clinical Sign | Risk Indicator |
|---|---|
| Bleeding on probing | Early sign of peri-implantitis |
| Pus or exudate | Active infection in peri-implant tissue |
| Radiographic bone loss > 2mm | Requires intervention |
| Halitosis or taste change | May signal anaerobic infection |
Without enough supporting bone, implants cannot integrate or stay stable over time.
Forces beyond what the implant can tolerate often lead to biomechanical failure.
✅ Monitoring risk factors reduces long-term failure – TRUE
explanation: early detection of loading, inflammation, or bone conditions allows intervention before failure progresses.
❌ Implant failure is usually caused only by surgical errors – FALSE
explanation: many failures result from occlusion, hygiene, prosthetic issues, and long-term maintenance gaps.
Implant failure isn’t always surgical. Prosthetic misfits, material fatigue, or retention issues can compromise long-term success. Understanding how lab-related and restorative design factors influence outcomes helps prevent complications and rework.

Prosthetic factors in implant failure
A restoration that doesn’t fit passively can cause stress at the implant-bone interface.
Residual cement is a hidden but frequent cause of peri-implant inflammation.
| Risk Factor | Complication |
|---|---|
| Excess cement beyond margin | Causes soft tissue irritation and inflammation |
| Subgingival margins | Make cement removal difficult or incomplete |
| Radiolucent cements | Prevent early detection in follow-ups |
| Lack of venting holes in crown | Increases risk of extrusion during seating |
Screw loosening can lead to instability, movement, or even fracture.
Material selection matters, especially in high-load zones or bruxing patients.
Lab-related complications such as poor fit, torque errors, and cement retention are often underestimated. These are not minor technicalities—they directly impact implant longevity. When labs and clinicians work in sync, long-term outcomes become more stable and predictable.
Early diagnosis is key to preventing full implant failure. Subtle signs—if monitored regularly—can reveal functional or biological issues before they become irreversible. A structured follow-up and documentation protocol can help clinicians act proactively.

Monitoring for implant failure
X-rays remain the most effective tool to detect peri-implant bone changes.
Soft tissue changes often signal early inflammation before structural failure sets in.
| Measurement | Clinical Concern |
|---|---|
| Probing depth > 5mm | Suggests tissue breakdown or infection |
| Bleeding on probing | Early indicator of peri-implantitis |
| Pus formation or halitosis | Points to active infection |
| Tissue color change or swelling | Indicates chronic inflammation |
An implant should never move under function. Any sign of mobility calls for immediate investigation.
Patient-reported issues are often the first clues. Don’t dismiss subtle complaints.
Early signs are easy to miss, but structured monitoring makes a difference. Diagnosis shouldn’t begin at failure—it should be part of every maintenance visit.
Coordinate with Raytops Dental Lab when unexpected issues arise for support with imaging review, prosthetic fit checks, and remake documentation.
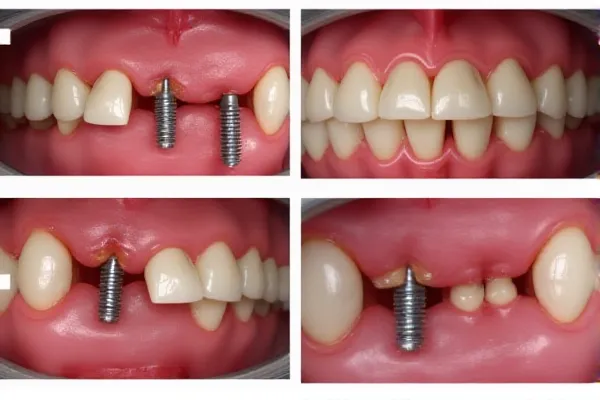
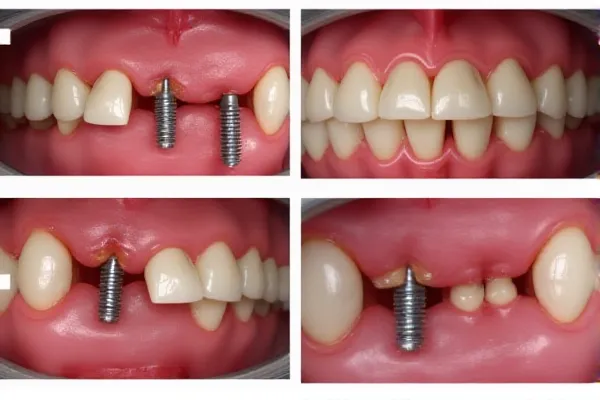
When implants fail, timely and appropriate clinical intervention can help preserve the site and restore function. Solutions depend on the cause and severity—ranging from conservative management to full explantation and rework. A clear protocol ensures the right decision at the right time.

Explantation and Site Regeneration Protocols
In cases of complete failure, removing the implant and rebuilding the site is necessary.
Failures related to cement retention or retrievability can be addressed through restorative redesign.
| Problem | Clinical Response |
|---|---|
| Residual cement causing inflammation | Shift to screw-retained to avoid subgingival cement |
| Need for frequent retrieval or repair | Screw-retained allows non-invasive access |
| Lack of vent or control during cementation | Eliminated with screw-based retention |
In peri-implantitis or soft tissue breakdown, infection control is essential.
When re-implantation is needed, guided planning improves accuracy and confidence.
✅ Re-treatment is more successful with digital planning – TRUE
explanation: guided re-entry with cbct and lab-supported planning improves precision and reduces risk.
❌ Implant failure always requires full replacement – FALSE
explanation: many cases can be managed with repair, redesign, or conservative intervention when caught early.
Preventing implant failure starts long before surgery. From careful case selection to long-term hygiene, each step matters. A structured, proactive system reduces avoidable complications and protects both clinical outcomes and patient trust.

Preventing implant failure
Not every patient is an ideal implant candidate. Screening for systemic, anatomical, and behavioral risks reduces early failure.
Surgical consistency protects against contamination and overloading.
| Step | Impact |
|---|---|
| Pre-op chlorhexidine rinse | Reduces bacterial load during placement |
| Two-glove sterile technique | Prevents intra-surgical contamination |
| Delayed vs. immediate loading decision | Avoids stress during healing |
| Multi-unit splinting in full arch | Distributes force, lowers micro-movement risk |
Restorative failure is often traced back to inconsistent lab standards.
Even a perfect surgery can’t survive poor hygiene. Maintenance is non-negotiable.
✅ Strict hygiene maintenance is optional once the implant heals – FALSE
explanation: long-term success depends on ongoing cleaning, monitoring, and risk management.
❌ Partnering with a qualified lab helps reduce failure risk – TRUE
explanation: consistent lab standards improve fit, reduce error, and align with clinical protocols.
Implant failure isn’t inevitable—it’s manageable with knowledge, systems, and vigilance. By identifying risk factors early, improving lab-clinic coordination, and implementing structured follow-up protocols, clinics can reduce complications and protect patient trust.
Need help reviewing complex cases or planning restorations to minimize risk?
[Contact Raytops Dental Lab] to access digital planning support, prosthetic fit verification, and failure-reduction workflows tailored for implant-heavy practices.