
Dental implant restorations are highly predictable—but they’re not immune to failure. Whether due to mechanical breakage, esthetic misalignment, or biological complications, restorations occasionally need to be redone. A clear remake policy helps clinics respond swiftly, protect their reputation, and manage patient expectations effectively.
An implant restoration failure is manageable when clinics have clear remake protocols, defined lab responsibilities, and transparent communication with patients.
From our perspective here at the lab, when a restoration comes back to us, it often falls into a few key categories. While the clinician sees the issue chairside, we analyze the component itself—the chips, the fit, the screw channel. Here’s how we classify the types of failures we most commonly encounter

Classification of implant restoration failure types
We analyze fractured pieces under magnification. Often, we can tell if the fracture originated from a design stress point that we might have queried with the clinic during planning, or if it’s purely due to excessive occlusal force or parafunction beyond the material’s limit.
✅ Restoration failure can arise from mechanical, esthetic, or biological issues – TRUE
Explanation: Understanding the type of failure helps determine if the issue is clinical, lab-related, or patient-driven.
❌ Once the implant is integrated, the restoration never fails – FALSE
Explanation: Restorative failures are possible years after successful integration.
Based on the remakes we receive and the clinical cases we help plan, we’ve compiled a list of the most common culprits behind restoration failures. It’s often a combination of factors, and understanding the root cause from both the clinical and technical sides is crucial for prevention.
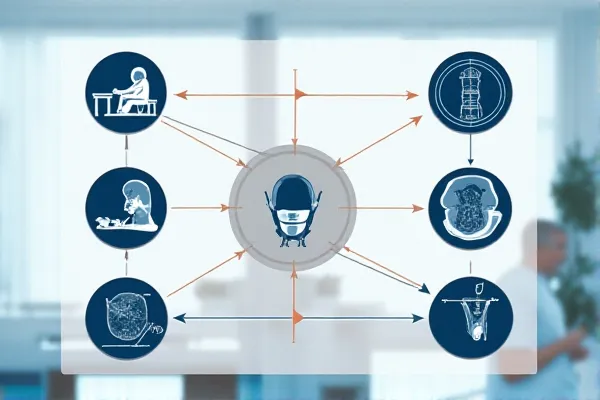
Implant failure root causes chart
Detecting issues like overmilled margins requires meticulous post-milling quality control at our end. We use specialized scanning and visual checks against the design file because we know that a microscopic misfit can lead to clinical issues down the line.
| Lab Error | Potential Complication |
|---|---|
| Overmilled zirconia coping | Increased fracture risk |
| Open contact area | Food impaction, drifting teeth |
| Under-polished margins | Gingival irritation, poor hygiene |
✅ Failures are often preventable through proper planning and communication – TRUE
Explanation: Most failures trace back to planning gaps, poor fit, or unmanaged risk factors.
❌ Failure causes are usually random and untraceable – FALSE
Explanation: Each failure is typically linked to a specific procedural or technical cause.
A clear, fair remake policy is essential not just for the clinic, but for us at the lab too. It eliminates ambiguity, streamlines the process, and helps us maintain a strong partnership. From our experience processing many remakes, here’s what makes a policy truly effective.

Dental remake policy document with eligibility terms
✅ A written remake policy protects both clinic and lab from disputes – TRUE
Explanation: Defined rules improve turnaround and clarify remake responsibilities.
❌ Remake criteria can be handled verbally on a case-by-case basis – FALSE
Explanation: Informal remake handling leads to delays and confusion.
The first thing we do is pull up the original scan and design file. We compare it against the failed restoration and any photos provided. Was the original margin design too thin? Did the scan capture the implant position accurately? This is our internal detective work.

Dental technician analyzing remake request
| Issue Observed | Responsible Party |
|---|---|
| Over-contoured crown | Lab (design error) |
| Incorrect cement technique | Clinic |
| Missing patient documentation | Shared or denied case |
✅ Lab remake review follows structured documentation and criteria – TRUE
Explanation: File review ensures quality control and fair decision-making.
❌ Labs must remake any failed crown regardless of the cause – FALSE
Explanation: Labs only remake if the failure is within scope and proven.
As a lab committed to quality, we welcome clinics asking about our QA steps. Ask us about our milling machine calibration logs, our post-milling inspection protocols, and how we verify passive fit before sending the restoration. That transparency is key to a trusting partnership.

Implant restoration QA checklist
While torquing is a clinical step, we understand its critical importance for restoration longevity. Our design process aims to create abutment/restoration interfaces that facilitate correct torque application and minimize stress on the screw/cement interface, but accurate clinical execution is vital.
✅ Proactive protocol adherence drastically reduces restoration failure – TRUE
Explanation: Workflow discipline and risk screening lead to fewer remakes.
❌ Failure risk cannot be lowered regardless of technique – FALSE
Explanation: Most failure points are preventable through planning and execution.
Setting expectations early prevents conflict if issues arise later.
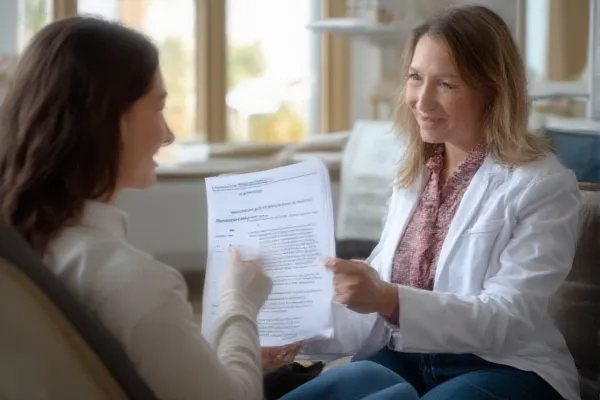
Clinician explaining remake clause to patient
✅ Proactive communication builds trust and reduces remake stress – TRUE
Explanation: Informed patients are less likely to panic if something breaks.
❌ Avoid mentioning remakes to maintain confidence – FALSE
Explanation: Surprise issues without preparation damage trust more than honesty.
As a lab, our goal isn’t just to mill a beautiful crown; it’s to be your partner in preventing the headaches of remakes. We build quality control and technical consultation into every case because we know that minimizes chair time and patient issues for you, and reduces costly remakes for everyone.
Take the Next Step
Need help creating your clinic’s remake policy or staff training guide? We can provide templates, consent forms, and technician-friendly SOPs to streamline your entire restoration workflow.