Not all crown & bridge labs are prepared to meet the diverse demands of today’s clinical workflows and patient preferences.
Labs limited to a narrow material range or lacking documentation often force clinics into compromises—either on esthetics, budget, or safety.
By evaluating material variety, digital compatibility, clinical adaptability, and sourcing transparency, you can partner with a lab that enhances both treatment flexibility and operational confidence.
A dental lab should provide a full range of crown and bridge materials, including full-contour and layered zirconia, lithium disilicate, PFM, hybrid ceramics, and metal alloys like nickel‑chromium or cobalt‑chromium. It should support digital workflow compatibility, offer tiered pricing structures, and supply documentation such as batch numbers, CE/FDA certificates, and biocompatibility reports.
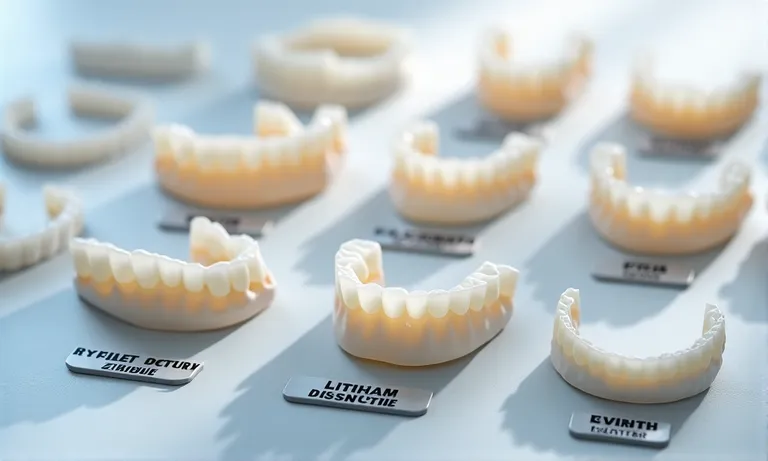
Crown & bridge labs must offer a complete material portfolio to serve the full range of clinical indications. From strength-demanding posterior units to esthetic anterior veneers, having access to multiple materials allows dentists to choose restorations based on both function and appearance.
Dental-Crown-Bridge-Materials-Zirconia-PFM-LithiumDisilicate
Modern labs typically stock:
A broad material base ensures readiness for different case types.
Material form impacts strength, esthetics, and price.
| Type | Strength | Esthetics | Use Case | Notes |
|---|---|---|---|---|
| Monolithic zirconia | ★★★★★ | ★★☆☆☆ | Posterior | Low wear, opaque |
| Layered zirconia | ★★★★☆ | ★★★★☆ | Anterior | Balanced, more lifelike |
| Lithium disilicate | ★★★☆☆ | ★★★★★ | Veneers/Inlays | Best esthetics, fragile in bridges |
Choosing the right type depends on indication—not just preference.
When a lab stocks and works with a complete material spectrum:
Material flexibility means clinical agility—and higher lab reliability.
✅ A full material range enables better case adaptation and client fit – TRUE
Clinicians can match indication to the best-performing material without workflow disruption.
❌ Zirconia alone covers all crown & bridge needs – FALSE
While versatile, zirconia lacks the esthetic nuance or flexibility needed for many anterior or hybrid applications.
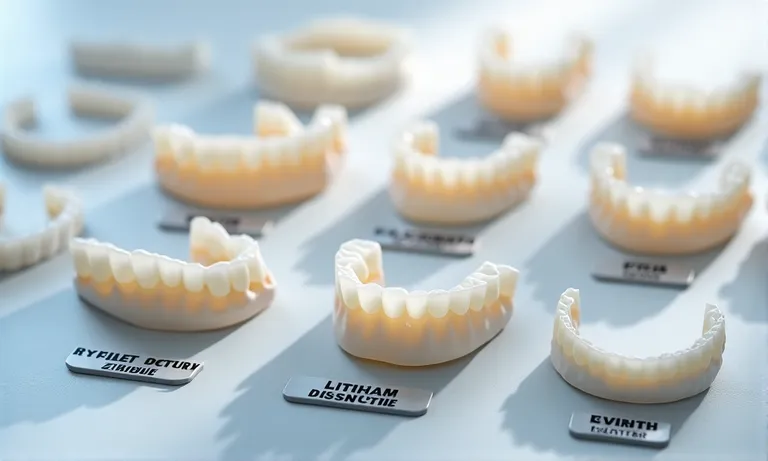
Not all materials suit every case. A crown & bridge lab must understand which materials best fit specific clinical scenarios—balancing strength, esthetics, and case complexity—to support better treatment outcomes and reduce adjustments or remakes.

Dental-Crown-Material-Clinical-Scenario-Matching
The restoration zone determines key material priorities:
Material selection here is about visibility, loading, and patient esthetic demand.
Different indications come with distinct material needs:
Choosing based on clinical indication reduces technical compromise later.
Some cases require hybrid decision-making between beauty, strength, and risk.
Good labs help clients find the right compromise—not just default to one material.
A material is only ideal when it suits both the clinical and functional needs of the case. Contact us for our clinical indication–material pairing chart to plan your next case with more clarity.
Crown & bridge labs that serve diverse clients—from private clinics to DSOs—must offer tiered material options. This enables clients to select restorations that fit clinical needs and patient budgets without compromising safety or reliability.

Dental-Crown-Material-Tier-Cost-Comparison
Each material comes with a distinct cost profile:
| Material | Estimated Cost Tier | Strength | Esthetics | Common Use |
|---|---|---|---|---|
| Gold or precious alloys | $$$ (high) | ★★★★☆ | ★★☆☆☆ | Full-cast crowns, PFM |
| Lithium disilicate (E.max) | $$ (medium) | ★★★☆☆ | ★★★★★ | Veneers, anterior crowns |
| Full-contour zirconia | $ (value) | ★★★★★ | ★★★☆☆ | Posterior units, bridges |
This comparison helps dentists balance case needs with budget sensitivity.
Some restorations combine esthetics with budget efficiency.
These options help clinics avoid costly upgrades when not clinically needed.
Tiering supports flexibility across client types and regions:
Smart labs don’t just offer one material—they offer structure.
✅ Tiered material options enable cost alignment without compromising safety – TRUE
With proper planning, labs can help clients meet budget needs using clinically sound materials.
❌ Lower-priced materials always mean lower quality – FALSE
Many modern materials like full-contour zirconia offer excellent performance at accessible pricing.
Material-specific design parameters must be integrated into the digital workflow for a crown & bridge lab to deliver accurate, consistent results. Each material—zirconia, lithium disilicate, PFM—has its own requirements for thickness, margin, and process type. Labs that pre-calibrate their CAD and milling settings help reduce chairside adjustments and remakes, as shown in a systematic review on digital vs conventional workflows that emphasizes precision and consistency across material-specific settings.
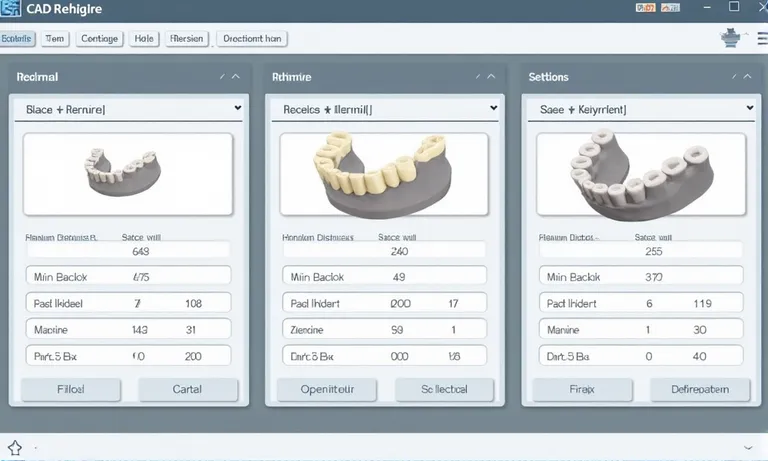
CAD-Material-Settings-Dental-Lab-Zirconia-Lithium-PFM
Each material has its own design thresholds:
Applying the correct parameters in CAD ensures proper strength and fit.
Labs must adjust design strategy based on restoration type and processing method:
Wrong design workflows increase fracture risk and reduce long-term survival.
Material planning must align with scanner output and design platform settings:
Labs familiar with this integration reduce need for chairside adjustments.
Digital workflows are only effective if aligned with each material’s structural and esthetic requirements. Proper calibration at every step—design, scan, and CAM—ensures your restorations arrive functional and predictable.
Labs must be able to demonstrate that all materials used in crown & bridge restorations are safe, traceable, and approved for dental use. Clear documentation builds trust with clients and regulators—especially when cases cross international borders.

Image
ALT: Dental-Material-Compliance-Documentation-Batch-Labels
Prompt:
A highly realistic, ultra-detailed, professional-quality image showing dental lab compliance documents neatly arranged on a clean countertop: including batch number labels, certificates of origin, FDA/CE certificates, and SDS (Safety Data Sheets). A technician’s gloved hand is organizing the files. Soft daylight highlights the details and clarity.
Every material should be fully traceable:
Traceability protects both the clinic and patient in case of quality disputes.
Regulatory documents should be aligned with export market:
Clients should confirm these certificates are valid and matched to the correct product type.
Labs should provide supporting material safety documentation:
This transparency supports compliance in audits, tenders, and recordkeeping.
Reliable labs integrate compliance into their daily workflow—not just during inspections. Request our material audit pack to verify every crown & bridge restoration meets international safety and documentation standards.
Crown & bridge material capability is more than a product list—it’s a reflection of how well a dental lab can support case diversity, patient expectations, and regulatory responsibility. Labs that offer material flexibility, digital readiness, and documentation transparency position their clients for both clinical precision and operational scale.
To explore how Raytops Dental Lab aligns material variety with digital design and regulatory fit, contact our case coordination team here.